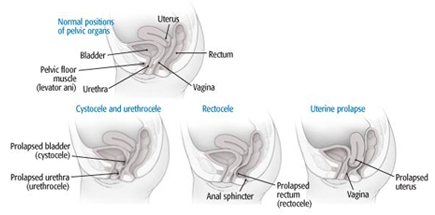
Pelvic organ prolapse (POP) occurs when there is a weakness or laxity in the supporting structures of the bladder, urethra, rectum, or uterus. When there is a lack of support, one or more of these organs can drop down, bulge, or prolapse into the vagina. The organ may also begin to exit out of the vagina. The support structures for these organs include the pelvic floor muscles, pelvic ligaments, and connective tissue or fascia. There are several types of prolapses. A prolapse of the bladder is called a cystocele and the urethra prolapse is referred to as a urethrocele. A rectocele occurs when the rectum prolapses into the vagina. Lastly, when the uterus descends into the vagina due to loss of support, it is referred to as a uterine prolapse. Causes of POP include childbirth with excessive pushing during delivery, multiple vaginal births, trauma or defect of the pelvic floor muscles, connective tissue disorders, menopause, obesity, hysterectomy, muscle tone loss with aging, excessive coughing, frequent bearing down due to constipation, and genetics. Symptoms may include pressure sensation or fullness in the vagina, sensation of a bulge in the vagina, pelvic discomfort, urinary or fecal incontinence, urinary urgency, painful intercourse, pulling or pain in the groin region, or constipation.
How can Pamela Morrison Physical Therapy, P.C. help with Pelvic Organ Prolapse?
Your expert pelvic physical therapist takes an extensive medical and pelvic history and then performs a thorough orthopedic and pelvic floor muscle exam. The pelvic floor muscle exam includes close inspection of the function and strength of the pelvic floor muscles. The prolapse(s) are graded (1 to 3) for severity. Grade 1 indicates a minor prolapse; Grade 2 indicates a moderate prolapse whereby the organ has descended close to the vagina opening; Grade 3 defines a severe prolapse: the organ has prolapsed outside of the vagina. Grade 3 requires surgical intervention, however, physical therapy is recommended post-surgically to restore normal function of the pelvic floor muscles. This prevents other pelvic organ prolapses from occurring and protects the surgical repair. Pelvic alignment is carefully assessed as well as pelvic connective tissue integrity. Your rehabilitation program can consist of pelvic realignment mobilization techniques, pelvic floor muscle rehab, postural re-education, neuromuscular re-education, pelvic support belts or garments, surface EMG pelvic floor muscle biofeedback, bowel/bladder retraining, prescriptive therapeutic exercises, and internal pelvic floor muscle electrical stimulation. Use of a temporary pessary (small removable device that supports a prolapse within the vagina) may be employed. We have a huge success rate with all types and grades of prolapses at Pamela Morrison Physical Therapy.


