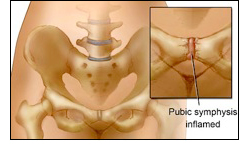
Osteitis pubis is a disorder of the pubic symphysis joint characterized by pain and inflammation of the joint and surrounding muscles such as the adductor group. Symptoms can include pain in the groin, lower abdomen, hip, perineum, bladder, clitoris, vagina, scrotum or testicles, and painful intercourse. It is most often caused by repetitive trauma or abnormal shearing forces to the pubic symphysis joint. Abnormal shearing forces can be caused by muscle imbalances, impaired flexibility, sacroiliac joint dysfunction, or a malalignment at the joint. When aggravating motions occur at the joint, microtrauma causes inflammation and muscle spasms can result. Other causes of osteitis pubis can be trauma from urogynecologic surgery, a motor vehicle accident or fall, sudden increase in exercise intensity, a leg length discrepancy, poor foot biomechanics, or poorly fitting shoes. This disorder is commonly seen in athletes. The pain increases upon kicking, changing directions or pivoting on one leg, jumping, and running. Sneezing or coughing, transferring from sitting to standing positions, and lying on one side can also exacerbate the pain. Clicking or popping may also occur at the joint upon walking or strenuous movements. Osteitis pubis can occur during pregnancy due to excessive pressure on the joint and release of the hormone called relaxin. Relaxin softens the ligaments at the pubic symphysis in preparation for childbirth perhaps leaving the joint susceptible to injury. Trauma from childbirth can worsen or bring on symptoms of osteitis pubis. Osteitis pubis can be a cause of pelvic floor muscle dysfunction if left untreated. An X-ray or CT scan can help with a proper diagnosis.
How can Pamela Morrison Physical Therapy, P.C. help Osteitis Pubis?
Your expert therapist at Pamela Morrison Physical Therapy, P.C. performs a complete evaluation including history and a full physical exam. Your therapist will examine spinal, pelvic, and lower extremity biomechanics and muscle function thoroughly to identify any malalignments and muscle impairments. The most important aspect of evaluating and treating this disorder is differentiating it from other disorders of the pubic symphysis such as a pubic symphysis separation, hernia, or groin strain. Treatment will consist of joint mobilization to realign the pubic symphysis and sacroiliac joints; modalities to decrease pain and inflammation such as therapeutic ultrasound, TENS, cryotherapy, iontophoresis, interferential electrical stimulation, cold laser; soft tissue mobilization or massage, cross-friction massage to the pubic ligaments, muscle rebalancing around the pubic symphysis joint, stability exercises, core and pelvic floor muscle re-education, correction of any faulty movement patterns or biomechanics, and pelvic support belts. Prescriptive therapeutic stretching and strengthening exercises will be instructed as part of a comprehensive program to prevent future injury. Pregnancy support garments may also be recommended. It may be recommended that you discontinue any exacerbating activity until symptoms improve. A home exercise program is given to all patients to facilitate a faster recovery.


