Interstitial Cystitis (IC): bladder pain syndrome, is a chronic inflammatory condition of the submucosal and muscular layers of the bladder. Interstitial cystitis presents as pain related to the bladder with urgency and frequency to urinate. There is also pelvic floor muscle dysfunction which involves overactivity, spasm, trigger points, shortening, and pain.
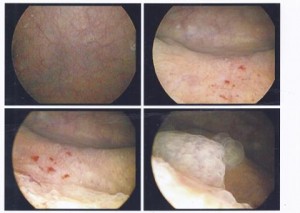
Here we observe my patient’s cystoscopy results. We are looking inside the bladder via a little camera. You see some red spots which are called glomerulations. Glomerulations are irritated blood vessels which produce tiny areas of bleeding in the bladder lining and is an indicator of Interstitial Cystitis. The patient has had Chronic Pelvic Pain for 10 years. 7 years ago this test was negative for any findings. He had not received proper diagnosis for awhile because many time IC signs may not show themselves until years after the symptoms begin making it frustrating for the patient to receive proper diagnosing and proper medical intervention. We advised to him to see another urologist for further testing when he came to see us earlier this year having failed with other interventions. He is now managing his IC pain with bladder instillations whereby medication is placed into the bladder and with our expert physical therapy. His symptoms are now 75% improved.
How can Pamela Morrison Physical Therapy help with IC?
A comprehensive physical therapy evaluation can determine if there is a musculoskeletal or neurological problem potentially causing or perpetuating the bladder and pelvic pain. Your musculoskeletal evaluation at Pamela Morrison Physical Therapy would determine if there are related joint problems, muscular problems such as pelvic floor muscle dysfunction, or nerve involvement in the pelvis, around the bladder area, and in surrounding structures. Your physical therapist may perform myofascial and trigger point release techniques to abdominal, hip, low back, and buttock muscles; nerve tension release techniques, and realign pelvic, sacroiliac, spine, and hip joints which may improve your symptoms or resolve them. Skillful visceral manipulation to the bladder and surrounding organs has truly proven to be an effective treatment approach in our clinic providing long term relief of symptoms. There are also other modalities such as electrical stimulation that may help calm the bladder and/or relieve pain. Use of physical therapy modalities such as interferential electrical simulation and TENS (transcutaneous electrical nerve stimulation) have been proven effective via research studies in treating patients with IC. Using real-time ultrasound and biofeedback enables the patient to understand the function of the pelvic floor muscles and low back muscles in bladder health. Specific exercises such as stretching, core stabilization, and pelvic floor muscle exercises aimed at down-training may be prescribed. Helping you to gain control of bladder habits and dietary/behavioral triggers is a crucial component of therapy. Sexual positions for improved comfort are also addressed.