Interesting Post Partum Case: Pubic Pain, Dyspareunia, Sacroliliac Joint Dysfunction, Diastasis Recti and the Biopsychosocial Model in Rehab
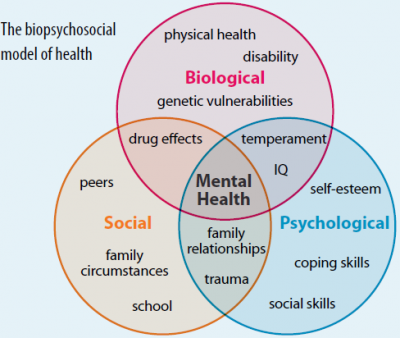
We evaluated woman today several months post partum and she primarily complained about pubic pain. It was her second vaginal delivery. During her first labor and delivery, she had to have only 1 suture from a minor perineal tear but was determined at this labor and delivery to not have any sutures. Her physician had recommended that when she was in labor with this second baby to not push even when her body was cuing her to do so. This “new approach” was to “let her uterus push the baby out” and help her keep an intact perineum. She had said that it felt wrong to not push while in labor when she had the urge but listened to her physician as it was to help her achieve the goal of no suturing, no tearing. She did experience vaginal labor and delivery but reported that the baby had been delayed exiting and felt stuck at the vaginal entrance. She still complied with the physician to not push. As a result, the baby did sit at the vaginal entrance for several minutes prior to the next uterine contraction which did inevitably help to push the baby completely out. She reported afterwards having moderate body shakes which felt like she was in shock or experiencing post traumatic stress disorder. Since the labor and delivery the patient has had pubic symphysis pain. She presented with a pubic symphysis shear (misalignment) yet no separation. Sitting cross-legged while nursing caused coccyx pain. She also had a sacral torsion/right sacroiliac joint dysfunction, generalized hypermobility, pelvic floor muscle dysfunction (pain, shortening, weakness) and dyspareunia (painful intercourse) from vulvar vestibulitis/allodynia. She is nursing so the redness and inflammation of the vulvar vestibule may be due to lower local tissue estrogen levels which is common for nursing mothers. However, upon questioning she did report always having penetration pain and painful insertion of tampons prior possibly revealing a pre-existing chronic vulvar pain condition. In addition, she presented with a 1.5 fingers diastasis recti at the umbilicus and above. After the evaluation we corrected her pubic symphysis alignment using advanced manual therapies to the hips and pelvic musculature followed by joint mobilization/muscle energy techniques. We educated her about her pelvic anatomy, what occurs at the pelvic joints and pelvic floor musculature during labor and delivery. We also corrected her habit of leg crossing in sitting and her nursing posture. We discussed the possible use of topical estrogen cream to the vulvar vestibule which she is to discuss with her referring physician. Upon the evaluation conclusion she was instructed to ice the pubis several times per day at home as this would surely help with pain and inflammation. She said that ice is not used in her culture and would not comply with that request and would rather have prolonged pain than use the ice for pain relief. With compassion and understanding we assured her that she would improve regardless of her ability to ice. We discussed whether she felt depressed or sad and also discussed the stresses of a new mother and how counseling may be beneficial. We had covered all of her concerns in this 1.5 hour session. She was given a home exercise program. She left feeling relieved. We are so looking forward to helping this patient achieve all of her rehab goals. This case is great example of using the biopsychosocial model in rehab. The biospychosocial model is an approach that considers biological, psychological (which entails thoughts, emotions, and behaviors), and social (socio-economical, socio-environmental, and cultural) factors. All play a significant role in human functioning in the context of disease or illness and addressing all of them will better help an individual resolve pain and recover.